by Richard J. Vahl and James B. Vahl
Information on this Web page is for educational use only, and is not intended as medical advice.
Every attempt has been made for accuracy, but none is guaranteed. If you have any serious health concerns, you should always check with your health care practitioner before treating yourself or others.
Always consult a physician before beginning or changing any fitness program.
Introduction
We consider the shoulder articulation unique because of its great degree of mobility throughout its entire range of motion. Popular throwing, racket, swimming, and gymnastics sports are especially demanding on this shoulder complex. Activities that are sport-specific for those sports place enormous and often excessive forces, wear, and stresses on the structures of the shoulder joint. Intense use, when combined with inadequate conditioning and incorrect body mechanics, is likely to result in an injury.
Discussion
The shoulder examination should be directed toward recognizing its dynamic dysfunction and finding sources of this dysfunction. Just as when dealing with any other joint, in order to recognize dysfunction of the shoulder the clinician must first have an understanding of its normal function. This understanding can be obtained only by studying normal shoulder anatomy and kinesiological function, including the role of even distant joints and muscles (parts of the kinetic chain) that influence the arm directly and through shoulder blade kinematics.
Shoulder Anatomy
Our focus in this paper is to identify structures that should be included in a routine examination of the shoulder. Those are:
— the glenohumeral, scapulothoracic, and acromioclavicular joints;
— soft tissue structures anteromedial to the glenohumeral joint, including the biceps and subscapularis, the coracobrachialis, and the major and minor pectoralis muscles;
— the interarticular (inside the joint) structures, including tendons of supraspinatus and infraspinatus and the very often injured or involved labrum, capsule, bursae, and ligaments;
— the posterior structures, including the scapula, rotator cuff, and scapular stabilizers; and
— the cervical and upper thoracic spine as well as the brachial plexus and its branches, the sternoclavicular joints, and related musculature (e.g., the paraspinals and scalenes).
Shoulder Biomechanics
For an in-depth discussion of the biomechanics of the shoulder, we refer the reader to our article titled Biomechanical Factors that Contribute to Rotator Cuff Dysfunction and Injury.
As previously mentioned, the complex shoulder articulation has a high degree of mobility throughout its range of motion. Any alteration or aberration in its mobility can put the shoulder at risk of reduced functional performance or injury.
Stability of the shoulder girdle is maintained primarily by the glenohumeral ligament complex, the glenoid labrum, negative intra-articular pressure, the compressive forces generated by muscles of the rotator cuff, and normal scapular kinematics as a part of the scapulohumeral rhythm. The scapula moves in coordination with the moving arm bone so that the instant center of rotation of the joint remains in what is considered the “safe zone.” Proper glenohumeral positioning and coordinated muscle activity maintain maximum concavity compression. Scapular retraction allows for the full “cocking” or “chambering” motion necessary for an explosive forward acceleration of the throwing arm. Scapular protraction allows for optimal glenohumeral positioning for deceleration in the follow-through motion.
Dynamic stability of the shoulder complex is of the utmost importance for all arm movements. Stability for the glenohumeral joint is provided by the coupled motions of the arm and scapula (scapulohumeral rhythm) throughout all the positions and movements permitted by a healthy shoulder. Optimal coupling of motions of the arm and scapula ensures acromial elevation, which prevents rotator cuff impingement. The optimal coupling/scapulohumeral rhythm (and thus sufficient acromial elevation) can be disrupted by fatigue of the serratus anterior, lower trapezius, and rotator cuff muscles. That is why we recommend that the examiner perform repetitive muscle testing (endurance testing) of these muscles as an important part of the shoulder evaluation.
The scapula is a link in the kinetic chain in which large forces are generated in the legs, hips, and trunk, then transferred through the spine to the scapula and the glenohumeral joint and ultimately to the arm and hand for execution of the throw, pass, serve, or punch. All this takes place while maintaining a stable scapular platform, which allows for the most appropriate shoulder function.
Evaluating the Shoulder
Taking the history is one of the most important parts of the evaluation. It must include the:
— mechanism of injury;
— location of pain;
— position(s) of the arm when pain or aggravating factors occur;
— position(s) of the arm when pain or aggravating factors are relieved;
— necessary activity modifications;
— history of prior injuries to the shoulder and kinetic chain structures;
— treatment update;
— sport-specific demands; and
— general medical history of the patient (general health, occupation, hand dominance, sports, leisure activities, family health).
As previously mentioned, functions of the proximal structures of the kinetic chain (i.e., legs, hips, and trunk) and the scapula are closely connected. A dysfunction or lack of strength of, say, pelvis stabilizers, forces compensations up the trunk, which may result in harmful alterations in function of shoulder blade stabilizers. Strength deficiencies of muscles stabilizing the pelvis and vertebral column are revealed in positions and movements that challenge one-legged stability: the one-legged stance, one-legged squat, and step-up/step-down. The examiner should look for an inability to keep hips level and square, specifically the following:
— Trendelenburg’s sign—when the person being tested is unable to maintain the pelvis relatively horizontal to the floor while standing on one leg. If the hip is normal, the iliac crest may be even or low on the standing (weight-bearing) leg side and high on the side of the lifted (non-weight-bearing) leg. If abnormal, the iliac crest will be high on the standing-leg side and low on the side of the lifted leg.
— Pelvic rotation—a twist in a horizontal plane (often accompanied by a compensatory vertical rotation of the pelvis, which can be symmetrical or asymmetrical)—a sign of an imbalance in activity of muscles of the pelvis that forces unwanted compensations up the trunk’s kinetic chain and thus adversely affects the shoulder blade.
— Corkscrew or winding posture—when there is a twisting-like spiral tendency in vertical posture.
— Forward lean—many individuals, especially bodybuilders, develop what we term a “flexion deformity”—an overdevelopment of the main flexor muscles on the front of the upper body. This can also be accompanied by an imbalance of the hamstring and quadriceps development. These cause a forward lean of posture accompanied by forward rounded shoulders and often a forward head carriage. A sitting lifestyle at school, work, and leisure also contributes to this type of posture, which among other things adversely affects shoulder function and development.
— Opposite-foot touch-down—unequal weight bearing and touch-down. While standing or moving, both feet should bear approximately the same weight and have equally solid touch-down. (We even use bilateral scales to help determine the weight bearing because we need more specific information to assist our spinal biomechanical evaluation, corrective treatment approach, and revaluation of progress).
— Increased lumbar lordosis (swayback)—usually accompanied by a compensatory excessive thoracic kyphosis (hunching), which weakens scapular retractors.
— Valgus knees (knock-knees)—usually caused by weakness of the sartorius, gracilis, and hip abductors.
Generally, these signs suggest weakness of the core muscles (the abdomen, back, and hips), which is why we consider these one-legged stability tests an important part of this evaluation.
Trunk flexibility can be assessed by asking the patient to perform forward and side bending movements. Functional stress X-ray films can be of benefit in conducting segmental evaluation of these important kinematic structures.
The patient’s cervical and thoracic posture should be assessed as well. These structures should be evaluated for things like thoracic scoliosis or excessive kyphosis and excessive cervical lordosis or cervical kyphosis. The soft tissues must also be evaluated, looking for tenderness and trigger points on palpation of the:
— spinous process regions,
— paraspinal region,
— levator scapulae,
— medial scapular border,
— rotator cuff musculature,
— serratus anterior,
— coracoid process, specifically the muscles that originate on the coracoid process (pectoralis minor, coracobrachialis, and short head of biceps) and ligaments that join it to the acromion, the clavicle, and the humerus,
— pectoralis minor and major, and
— biceps tendon (tendon of the long head of the biceps brachii).
Examining Shoulder Muscle Strength
Supraspinatus strength is assessed by resisted arm abduction in the scapular plane (the plane at about 30 degrees between the frontal plane and the sagittal plane—to find it raise your arm to the side and then bring it forward 30 degrees).
Infraspinatus strength is tested by resisted external arm rotation with the elbow at 90 degrees with the arm at the side. For both these tests the scapula must be retracted so it can provide a stable base for muscle action.
Subscapularis strength can be tested with the “belly test” (by internally rotating the arm and pressing the hand into the belly); with the “lift-off test” (internally rotating the arm and lifting the hand off the back against resistance); and by doing an uppercut type of maneuver against resistance. This last test can also be used to assess biceps muscle strength.
Measuring Shoulder Range of Motion
The shoulder range of motion should be examined in arm flexion, abduction, and internal and external rotation at 0 and 90 degrees. It is important to pay particular attention to the presence of glenohumeral internal rotation deficit, or GIRD, which can be associated with labral and rotator cuff injury in throwers and in racket-sports players. GIRD assessment can be done by comparing side-to-side differences in internal rotation, measured using a goniometer. For the measurement, the scapula must be stabilized and the shoulder abducted to 90 degrees and then internally rotated to the point of tightness.
Importance of arm position in evaluating scapular dyskinesis (an alteration in the normal position or motion of the shoulder blade during arm movements): The scapular position can reveal the cause of scapular dyskinesis. Scapular “winging” as well as abnormalities of translation (shifting or gliding) and rotation should be assessed at rest and during arm abduction and flexion. Muscle weakness causing scapular dyskinesis manifests itself often as a “jump,” “clunk,” or “catch” (similar to what is often felt in shoulder multidirectional instability), especially in the descending phase of arm movement. The dyskinetic pattern can be classified based on the position as one of three types:
Type 1—the inferomedial border is lifted (due to lower trapezius weakness)
Type 2—the medial border is lifted (due to serratus anterior weakness)
Type 3—the superomedial border is lifted (due to upper trapezius weakness)
However, we often find dyskinesis in more than one plane, so it is important to identify all the dyskinetic patterns.
Further Evaluations
Scapulothoracic bursitis (snapping scapula)—confirmed if arm abduction elicits painful crepitus over the superomedial or inferomedial borders of the shoulder blade.
Scapular retractor weakness (mainly of rhomboideus minor and major)—confirmed if an isometric retraction of the shoulder blades (as if trying to pinch something between them) causes a burning pain within 15 seconds.
Serratus anterior strength—have the patient do 10 wall push-ups or incline push-ups. Either will do. We prefer the incline push-ups with hands on two fairly high chairs. However, wall push-ups are satisfactory as long as the feet are at least approximately 30 inches away from the wall, farther for very tall persons. If the person struggles to do 10, this is a sign of serratus anterior weakness.
Impingement
— Neer’s test is performed by elevating the arm through forward flexion with internal rotation while stabilizing the scapula. It detects degenerative changes that involve mainly the supraspinatus tendon, at times the anterior part of infraspinatus tendon, and occasionally the tendon of the long head of the biceps.
— Hawkins’ test is performed by flexing the arm to 90 degrees, bending the elbow 90 degrees, and then internally rotating the arm. It indicates impingement between the greater tuberosity of the humerus against the coraco-acromial ligament, trapping all structures that are there.
Both these tests are considered positive if pain is elicited while performing the maneuver.
— Scapular assistance test is performed to evaluate scapular and acromial involvement in the subacromial impingement (i.e., impingement due to poor or late acromial elevation). Stabilize the superior border of the shoulder blade and then assist the inferior border to facilitate upward rotation, posterior tilt, and external rotation of the scapula during elevation of the arm. These actions stimulate the normally coordinated activity of the serratus anterior and lower trapezius muscles. Elimination or just a reduction of impingement symptoms through this procedure indicates that rehabilitation should focus on these muscles.
— Scapular retraction test is performed to evaluate internal impingement (i.e., impingement due to the excessively protracted position of the scapula, which makes it difficult for the rotator cuff muscles to stabilize the humeral head in the glenoid cavity). Stabilize the scapula in a retracted position on the thoracic wall, as this position provides a stable base of origin for the rotator cuff muscles and will often improve supraspinatus strength. It may also decrease pain related to internal impingement. Increased supraspinatus strength and pain reduction indicate that rehabilitation should focus on strengthening the rhomboids and trapezius.
Scapular Stabilizer Strength
— Lateral scapular slide test gives a quantitative measurement of strength of scapular stabilizers. This test compares the position of the scapula in the injured and noninjured side in relation to a fixed point in three different arm positions:
— Arms at the side
— Arms akimbo, hands on the hips with the fingers anterior and thumb posterior, with about 10 degrees of shoulder extension
— Arms at 90 degrees of flexion, with maximal internal rotation of the glenohumeral joints
In each of these arm positions, the distance between the inferior angle of the scapula and a fixed bony point on the spine is measured on each side. A side-to-side difference of 1.5 cm or more in any of these positions is considered abnormal.
Labral Pathology
The following tests reveal labral pathology if they cause pain or crepitus (joint noises such as popping, grinding, or crackling).
The integrity of the glenoid labrum can be tested by palpating for tenderness along the anterior and posterior joint lines while moving the glenohumeral joint through its range of motion. Here are more tests of glenoid labrum integrity:
— The anterior slide test. The patient’s hand is on his or her hip, fingers anterior and thumb posterior, the arm in about 10 degrees of extension. The examiner pushes up on the elbow while the patient resists.
— O’Brien’s test. The patient’s arm is flexed 90 degrees, adducted 10-15 degrees medial to the sagittal plane of the body, and internally rotated so that the thumb points downward. The examiner pushes down on the elbow while the patient resists.
— Kim test. The patient’s elbow is flexed, arm abducted to 90 degrees and externally rotated. The examiner pulls on the forearm to extend the elbow while the patient resists.
— Mayo shear test. The patient’s arm is abducted to 90 degrees then passively externally rotated and pulled down. The examiner palpates the posterior joint line.
Glenohumeral Instability
The following tests reveal glenohumeral instability if they cause pain or there is increased joint laxity in comparison with the other, healthy shoulder.
— Anterior drawer test for anterior instability. The scapula is stabilized and the two sides compared. Then the arm is held and shifted forwards (translated anteriorly) to test for anterior instability.
— Posterior drawer test for posterior instability. The scapula is stabilized and the two sides compared. Then the arm is held and shifted backwards (translated posteriorly) to test for posterior instability.
— Sulcus test (sulcus = groove) for inferior instability. The scapula is stabilized and the two sides compared. Then the arm is pulled down (distracted inferiorly) to create a sulcus (groove) between the acromion and the humerus.
Clavicle Function
The importance of proper clavicle function in evaluating shoulder dysfunction: In our opinion, one of the most overlooked and misunderstood areas of shoulder dysfunction can be due to misalignment and aberrant clavicle biomechanics and function. In addition to clavicle subluxations and separations of the acromioclavicular articulation and subluxations of the sternoclavicular articulation, the often overlooked evaluation of the kinematics function and rotation of the clavicle is of the utmost importance.
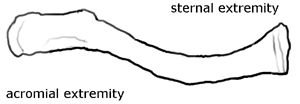
Clavicle
The clavicle is shaped like a shallow “S.” The reason for that “S” type configuration is that it allows the clavicle to function like a “crank” when the arm is raised or lowered. When the arm is raised the clavicle should rotate superiorly, and when it is lowered it should rotate inferiorly. These movements are very important and necessary for proper biomechanical function of the shoulder complex. Therefore, proper clavicle function should be examined and evaluated as a part of shoulder girdle examination and function. If the clavicle is subluxated, is misaligned, or lacks proper rotation as described, it can affect the dynamic function of the entire shoulder girdle complex and even cause misalignment and injury to not only the clavicle articulations but other shoulder structures as well. It can also affect shoulder kinematics and performance. This area is often one of the most overlooked areas of the important kinetic chain.
Conclusion
As we have discussed, to determine causes of shoulder dysfunction, pathomechanics, or pathology, it is necessary to obtain the patient’s history and perform a thorough and exact physical and functional examination. As we have learned, the examination should be of not only the shoulder joint but also the entire shoulder girdle complex including the scapula, clavicle, and proximal kinetic chain structures, down to the feet. This approach is the only one for making an accurate diagnosis, which forms the basis for designing an effective postinjury rehabilitation, or better yet, an injury prevention program for the patient.
* * *
Dr. Richard J. Vahl
is a former professor and department chairman at the Palmer College of Chiropractic in Davenport, Iowa. He is an Adjunct Emeritus Professor on the ICA Council on Fitness and Sports Health Science. In addition to his DC degree, he has a Ph.D. in Health, Physical Education and Sports Science. He is a diplomat of the American Academy of Pain Management and a fellow in Applied Spinal Biomechanical Engineering. Dr. Vahl is a Certified Master of Fitness Science and Sports Science by the International Sports Sciences Association (ISSA). He has published and lectured both nationally and internationally and is a member of the National Association for Sport and Physical Education (NASPE) and the National Academy of Sports Medicine (NASM). He has been a team doctor for many state, national, and international sporting and martial arts events and has been the team doctor and medical advisor for the USA Kendo Team and Team Miletich Fighting Arts.
James B. Vahl, BSc, DC,
is a graduate of San Diego State University (SDSU) in Pre-Professional Health Care, Molecular Biology and Sports Medicine. Following a career as a published DNA researcher for Applied Bio Systems, Dr. Vahl earned his Doctorate of Chiropractic with special high honors from Palmer College of Chiropractic in Davenport, Iowa. He is a Certified Practitioner in Active Release Techniques (ART), GRASTON Technique, and Extremity Injuries. He is also a Certified Professional Health and Fitness Specialist by the American College of Sports Medicine (ACSM) and a Certified Physical Trainer by the American Council on Exercise (ACE). Dr. Vahl is a member of the National Academy of Sports Medicine (NASM), and he is in private practice at Vahl Chiropractic Wellness & Sports Injury Center in Encinitas, CA.